[Disclaimer: I am an employee of Bristol Myers Squibb. The views expressed here are my own.]
One of my favorite questions to ask is: “What captures your imagination?” At a recent family dinner, responses were varied but encouraging for the next generation: black swan events, comparative anatomy & human physiology, space exploration & intelligent life beyond our planet, and more. My response was programmable therapeutics, a topic which I have blogged about in the past.
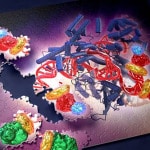
In this blog I define programmable therapeutics and provide a few recent examples (severe combined immune deficiency and mRNA vaccines). As you will see, programmable therapeutics is more than pure imagination – we are seeing this new concept evolve before our very eyes.
What is the concept of programmable therapeutics?
While there are different definitions of the concept of programmable therapeutics (see a16z talk; programmable cells; synthetic biology; CRISPR base editing), my definition of programmable therapeutics relates to a platform with modular components that can shorten the time from new target to drug candidate and ultimately regulatory trials that can lead to an approved medicine.
For most drug development programs, the identification of a drug target represents the start of a long journey that is highly artisanal.…
Read full article...
[Disclaimer: I am an employee of Celgene. The views reported here are my own.]
Drug research and development (R&D) is a slow, arduous process. As readers of this blog know, it takes >10 years and upwards of $2.5 billion dollars to bring new therapies to patients in need. An aspiration of the biopharmaceutical ecosystem is to shorten cycle times and increase probability of success, thereby dramatically improving the efficiency of R&D.
One potential solution is to use human genetics to pick targets, understand molecular mechanism, select pharmacodynamics biomarkers, and identify patients most likely to respond to treatment (see Science Translational Medicine article here). While intuitively appealing and supported by retrospective analyses (here), it is not yet routinely implemented in most R&D organizations (although see Amgen blog here; Regeneron study below). Indeed, human genetics often represents an inconvenient path to a new therapeutic, as it takes substantial effort to understand the molecular mechanism responsible for genetic risk and many such targets are difficult to drug.
But what if…
…it were possible to go from gene variant to therapeutic hypothesis instantly via in silico analysis;
…it were possible to select an “off-the shelf” therapeutic molecule that recapitulates a human genetic mutation, and take this molecule into humans almost immediately, with limited pre-clinical testing;
…it were possible to select pharmacodynamics (PD) biomarkers that capture underlying human physiology, and to measure those PD biomarkers in a small, human proof-of-mechanism clinical trial;
…it were possible to model the magnitude of effect of a therapeutic intervention relative to existing standard-of-care, and thereby to estimate the commercial market of an as-yet-to-be-approved drug?…
Read full article...

Last week Alnylam reported positive news on Phase 3 outcomes for their RNA interference (RNAi) therapy to treat patients with a rare genetic cause of amyloidosis with polyneuropathy (see here). I tweeted the following:
The 20-year journey from scientific discovery to positive Phase 3 clinical trial data got me thinking about other novel therapeutic modalities. Was twenty years a long time or typical for an innovative therapeutic modality? Where are other promising modalities on their journey to regulatory approval? Is the biopharmaceutical industry on the cusp of a series of innovative modalities that could change the therapeutic landscape for patients? How will these new modalities improve our ability to test therapeutic hypotheses?
[Disclaimer: I am an employee of Celgene. The views expressed here are my own.]
To explore these questions, I decided to review different novel therapeutic modalities, which I am defining as those other than small molecules, protein therapeutics (e.g., insulin) and traditional vaccines. This decision was practical, as the amount of literature in these modalities is expansive.
For each new modality, I asked whether a drug has been approved by either a European or US regulatory agency (EMA and FDA, respectively). If a drug has been approved, I reviewed the time from seminal scientific discovery (which sometimes is clear, sometimes is not) to the approved therapy.…
Read full article...

As readers of my blog know, I am a strong supporter of a disciplined R&D model that focuses on: picking targets based on causal human biology (e.g., genetics); developing molecules that therapeutically recapitulate causal human biology; deploying pharmacodynamic biomarkers that also recapitulate causal human biology; and conducting small clinical proof-of-concept studies to quickly test therapeutic hypotheses (see Figure below). As such, I am constantly on the look-out for literature or news reports to support / refute this model. Each week, I cryptically tweet these reports, and occasionally – like this week – I have the time and energy to write-up the reports in a coherent framework.
Of course, this model is not so easy to follow in the real-world as has been pointed out nicely by Derek Lowe and others (see here). A nice blog this week by Keith Robison (Warp Drive Bio) highlights why drug R&D is so hard.
Here are the studies or news reports from this week that support this model.
(1) Picking targets based on causal human biology: I am a proponent of an “allelic series” model for target identification. Here are a couple of published reports that fit with this model.…
Read full article...

Like many, I waited with bated breath for results of the anti-PCSK9 (evolocumab) FOURIER cardiovascular outcome study last week. There have been many interesting commentaries written on the findings. A few of my favorites are listed here (Matthew Herper), here (David Grainger), here (Derek Lowe), and here (Larry Husten), amongst others, with summaries provided at the end of this blog. Most of these articles focused on clinical risk reduction vs. what was predicted for cardiovascular outcome, as well as whether payers will cover the cost of the drugs. These are incredibly important topics, and I won’t comment on them further here, other than to say that the debate is now about who should get the drug and how much it should cost.
In this blog, I want to emphasize key points that pertain to human genetics and drug discovery. And make no mistake: the anti-PCSK9 story and FOURIER clinical trial outcome is a triumph for genetics and drug discovery. This message seems to be getting muddled, however, given the current cost of evolocumab and the observation that cardiovascular risk reduction was less than expected, based on predictions from a 2005 study published by Cholesterol Treatment Trialists (CTT) (see Lancet study here).…
Read full article...

Yesterday I participated in the National Academy workshop, “Enabling Precision Medicine: The Role of Genetics in Clinical Drug Development” (link here). There were a number of great talks from leaders across academics, industry and government (agenda here).
I was struck, however, by a consistent theme: most think that “precision medicine” will improve delivery of approved therapies or those that are currently being developed, whether or not the therapies were developed originally with precision medicine explicitly in mind. Many assume that the observation that ~90% medicines are effective in only 30% to 50% is the result of biological differences in people across populations (see recent Forbes blog here). This hypothesis is very appealing, as there are many unique features to each of us.
An alternative explanation is that most medicines developed without precision medicine from the beginning only work in ~30% patients because the medicines don’t target the biological pathways that make each of us unique.
I believe the most likely application is in the discovery and development of new therapies. That is, I believe that the greatest impact will come when precision medicine strategies are incorporated into the very beginning of drug discovery, and will only rarely have an impact on therapies that were not developed with precision medicine in mind from the start.…
Read full article...

A new sickle cell anemia gene therapy study published in the New England Journal of Medicine (see here, here) gives hope to patients and the concept of rapidly programmable therapeutics based on causal human biology. But how close are we really?
It takes approximately 5-7 years to advance from a therapeutic hypothesis to an early stage clinical trial, and an additional 4-7 years of late stage clinical studies to advance to regulatory approval. This is simply too long, too inefficient and too expensive.
But how can timelines be shortened?
In the current regulatory environment, it is difficult to compress late stage development timelines. This leaves the time between target selection (or “discovery”) and early clinical trials (ideally clinical proof-of-concept, or “PoC”) as an important time to gain efficiencies. Further, discovery to PoC is an important juncture for minimizing failure rates in late development and delivering value to patients in the real world (see here).
Here, I argue that rapidly programmable therapeutics based a molecular understanding of the causal disease process is key to compressing the discovery to PoC timeline.
Imagine a world where the molecular basis of disease is completely understood. For common diseases, germline genetics contributes approximately two-thirds of risk; for rare diseases, germline genetics contributes nearly 100% of risk.…
Read full article...
This week’s theme is genes to function for drug screens…with a macabre theme of zombies! As more genes are discovered through GWAS and large-scale sequencing in humans, there is a pressing need to understand function. There are at least two steps: (1) fine-mapping the most likely causal genes and causal variants; and (2) functional interrogation of causal genes and causal variants to move towards a better understanding of causal human biology for drug screens (“from genes to screens”).
Genome-editing represents one very powerful tool, and the latest article from the laboratory of Feng Zhang at the Broad Institute takes genome-editing to a new level (see Genetic Engineering & Biotechnology News commentary here). They engineer the dead!
Genome-scale gene activation by an engineered CRISPR-Cas9 complex, Nature (December 2014).
Since its introduction in late 2012, the CRISPR-Cas9 gene-editing technology has revolutionized the ways scientists can apply to interrogate gene functions. Using a catalytically inactive Cas9 protein (dead Cas9, dCas9) tethered to an engineered single-guide RNA (sgRNA) molecule, the authors demonstrated the ability to conduct robust gain-of-function genetic screens through programmable, targeted gene activation.
Earlier this year, the laboratories of Stanley Qi, Jonathan Weissman and others \ reported the use of dCas9 conjugated with a transcriptional activator for gene activation (see Cell paper here).…
Read full article...