[Disclaimer: I am an employee of Bristol Myers Squibb. The views expressed here are my own.]
One of my favorite questions to ask is: “What captures your imagination?” At a recent family dinner, responses were varied but encouraging for the next generation: black swan events, comparative anatomy & human physiology, space exploration & intelligent life beyond our planet, and more. My response was programmable therapeutics, a topic which I have blogged about in the past.
In this blog I define programmable therapeutics and provide a few recent examples (severe combined immune deficiency and mRNA vaccines). As you will see, programmable therapeutics is more than pure imagination – we are seeing this new concept evolve before our very eyes.
What is the concept of programmable therapeutics?
While there are different definitions of the concept of programmable therapeutics (see a16z talk; programmable cells; synthetic biology; CRISPR base editing), my definition of programmable therapeutics relates to a platform with modular components that can shorten the time from new target to drug candidate and ultimately regulatory trials that can lead to an approved medicine.
For most drug development programs, the identification of a drug target represents the start of a long journey that is highly artisanal. New screens are required to find chemical matter (small molecules or antibody fragments) that bind to a target of interest; bespoke assays are developed to measure biological activity in vitro; and animal models are created to estimate efficacy in a living organism. Once a drug candidate is identified, a new manufacturing process is developed to allow scale-up of material for toxicology studies and clinical trials. Discussions with government regulators start anew for each drug candidate, and clinical development begins the arduous march through safety & tolerability studies, dose selection, registrational trials, and (hopefully!) regulatory approval.
Each step along the way is highly customized, and a big idea can fail at any step along the way.
But is it possible to create a modular platform that simplifies as many of these steps as possible? And if so, will such a modular – or programmable therapeutic – decrease time and increase probability of success from new idea to an approved medicine?
In many ways the origins of programmable therapeutics can be traced to 1973 and the founding of Genentech, which used genetic engineering technology to introduce a gene sequence into bacteria cells to make human proteins such as insulin, growth hormone, and tissue plasminogen activator (here, here). The key advance was to transform the inefficient traditional method of making a drug (e.g., extracting them from plants and animals) to scale-up manufacturing in fermentation vats of microbes.
But advances today make the concept of programmable therapeutics even more exciting, as many more steps may be simplified. Furthermore, regulators are paying attention to how to evaluate these modular steps.
One of the first steps to be simplified is the choice of target, as advances in science have led to a much deeper understanding of causal human biology. Genentech was confident in its original target – human insulin – because insulin was already an approved therapy. Today, advances in human genetics (see gene therapy below) and human pathophysiology (see mRNA vaccine below) are helping to de-risk targets to the point where drug candidates that recapitulate causal human biology can be “inserted” into a deliver vector with limited pre-clinical studies to establish confidence in efficacy.
In the programmable therapeutics model, the delivery vector (e.g., lentiviral or AAV gene therapy, mRNA to encode proteins for vaccines) is key, as it is one component of the modular system that can be used again and again. As an active drug substance, the properties of a delivery vector remain identical from drug product to drug product. What does change is the payload that is inserted into the delivery vector.
However, if there is shared biology from one payload to the next across different drug products, then the amount of pre-clinical work to establish evidence for efficacy is greatly reduced.
Thus, the key components of a programmable therapeutic are:
(1) delivery vector that has been de-risked in terms of safety and has the capacity to easily scale for manufacturing;
(2) payload that can be packaged into the delivery vector to create a new drug product; and
(3) shared biology across multiple payloads, such that success for one delivery vector plus payload-X (drug product X) increases greatly the likelihood of success for the same delivery vector plus payload-Y & -Z (drug products Y and Z, respectively).
Primary immune deficiency
An example of programmable is ex vivo correction of gene defects responsible for primary immune deficiency, or PID (reviews here, here). The most severe form is referred to as severe combined immune deficiency, or SCID, which represents a severe, life threatening disorder that, if untreated, leads to increase risk of infection and death. Currently, allogeneic hematopoietic stem cell transplant (HSCT) represents a cure for ~60% of eligible patients with severe combined immune deficiency (SCID). Moreover, even those successfully treated suffer long-term consequences such as Graft vs Host Disease (GvHD).
An autologous stem cell transplant would create therapeutic options for all SCID patients – see recent NEJM article on ADA-SCID – but there needs to be a mechanism to correct the defective gene before returning a patient’s own cells in the form of a stem cell transplant (see Figure below). In 1990, the first patient with ADA-SCID patient was successfully treated with gene therapy. Strimvelis, the second gene therapy to be approved in Europe (2016), has clinical data to support the claim of 100% durable cure: >25 patients have been treated and followed for >15 years, and all remain cured. Unfortunately, concerns about insertional mutagenesis (Strimvelis is a gamma retrovirus) and challenges of access (Strimvelis can only be administered at a single hospital in Italy) has limited wide-spread adoption as frontline treatment for ADA-SCID.
Advances in viral (e.g., lentivirus – see figure) and non-viral vector technology now make it possible to safely insert a corrected copy of the gene, and then to transfuse these corrected cells back into the patient. Critical to the concept of programmable therapeutics, if his process is successful for one SCID genetic defect, it should be possible to scale this same approach to other SCID genetic defects.
What is particularly interesting is to look at the total number of PID (~350 genes mutated) and the number cured by allogenic transplant to estimate how many PID genes might be amenable to a programmable therapeutic approach. There are at least 15 SCID genes that could fit with the programmable therapeutics model. Thanks to support from organizations such as the Jeffrey Modell Foundation, newborn screening is now in place across all 50 states in the US and is set to roll-out in Europe within the next 5 years. Thus, it is now possible to identify patients who suffer from SCID early in life.
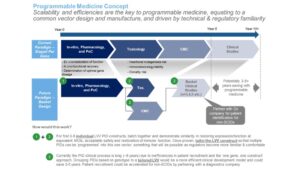
How might programmable therapeutics decrease time and increase probability of success for ex vivo gene therapy for SCID? First, identify all SCID genes amenable to correction with an autologous stem cell transplant. Based on the shared biology of these genes, it should be possible to create a highly-simplified pre-clinical system to test all these genes – and the corresponding gene therapy drug product engineered in a common lentiviral vector (LVV) – in parallel.
Second, initiate a common Chemistry, Manufacturing and Controls (CMC) and toxicology screening system based on the common delivery vector system and genetic payload that is biologically similar. By working directly with regulators, it should be possible to gain alignment on a CMC and toxicology package that can be utilized for the same delivery vector and different payloads, assuming that the payloads are sufficiently similar in terms of shared biology.
Third, design a clinical program where a basket of indications – SCID due to different gene mutations – is tested in one trial. SCID patients are rapidly identified through newborn screening T-cell receptor excision circles (TREC) assay and the defective genes are identified through next-generation sequencing. Grouping SCID patients by molecular mechanism should save several years in clinical development.
This framework, if successful, should demonstrate proof-of-concept of programmable therapeutics in a severe genetic disorder amenable to treatment with ex vivo gene therapy.
mRNA vaccines
The coronavirus pandemic has introduced the world to mRNA as a therapeutic modality. The story told today is that once the coronavirus sequence was published (January 11, 2020), an mRNA drug product was generated within 48 hours. While true – and certainly speaks to the power of programmable therapeutics – decades of research, with many failures, provided an opportunity for those famous 48 hours to be possible (e.g., 2P mutation to stabilize the prefusion form of a related coronavirus, MERS-CoV).
Equally remarkable, 42 days after the genetic code was released, a few hundred vials of the experimental vaccine was manufactured for clinical trials. And just 18 weeks and 2 days after the sequence was made public (May 18), positive interim clinical data was reported via a press release: the vaccine had generated neutralizing antibodies in the first eight volunteers tested.
Thus, in just over 4 months, a new idea was conceived (mRNA vaccine against the coronavirus spike protein) and tested in humans, with evidence of a biological activity that is highly predictive of an approved drug.
The power of programmable therapeutics extends beyond the initial discovery and development of the first SARS-CoV-2 mRNA vaccines. Naturally occurring mutations, or variants, in the SARS-CoV-2 spike protein are evolving, with concern that these variants may make first-generation vaccines less effective. Fortunately, mRNA technology allows for the rapid generation of booster shots for these variants, which are currently being tested in clinical trials.
Concluding remarks
The examples of ex vivo gene therapy in SCID and mRNA vaccines for SARS-CoV-2 provide compelling examples of progress being made. But there are other examples, too:
- – Genome editing with CRISPR/cas9 and related products (here, here, here, here)
- – Cell therapy against cancer targets (here)
- – Immune tolerance against known autoantigens (here)
- – Antisense therapeutics (here)
Moreover, investment is being made in manufacturing systems to scale production of the modular components required to realize the vision of programmable therapeutics.
Taken together, it is clear to me that the world of programmable therapeutics is upon us. It will take imagination, investment, and persistence to deliver medical innovation to patients in need.
“If you want to view paradise
Simply look around and view it
Anything you want to, do it
Want to change the world?
There’s nothing to it”
- – “Pure Imagination” Charlie and the Chocolate Factory